Founder Paul Lynch Fights COVID-19 In New York City at Bellevue Hospital
Dr. Lynch Helps Fight Coronavirus in NYC
WorldPix Founder, Dr. Paul Lynch, went to the epicenter of the COVID-19 pandemic. He decided he will document his time fighting the virus and “save as many lives as he can.” Our team is watching and summarizing his journey on this blog post so that others can get perspective on how the fight against this virus is going from our leader on the front lines. We are accepting donations to help those Paul is helping in these videos. Please donate and help us help Paul during the fight!
We are currently working with New York City Relief NPO where our Co-Founder, Dr. Paul Lynch is volunteering his time at the Bellvue Hospital ICU.
If you would like your donation to goto New York City Relief NPO please make note of that in your donation comments.
Thanks for everyone’s continued prayers and support at this crucial time.
Please donate today!
Day 1
Paul began the video explaining that he was nervous about not being able to help, he had to be fit tested and was worried about being sent home due to asthma, but he was cleared to help people. This was his first day, 6:30am-8:00pm and his first two patients of the day were gentlemen under the age of 41 that required extensive medical treatment, including having their blood removed to oxygenate before being returned. Even with this, one of the men had vitals that would not regulate. Paul learned a lot about PPE and washed his hands about 400 times.
Teaching point 1. This disease is very real
Teaching point 2. Paul was very impressed with the human spirit and people pulling together to fight this pandemic.
Day 2
Day 3
Day three of Paul Lynch working in New York City, in the ICU. He is exhausted from working about 14 hours today. It is basically a War Zone.
Paul explains a little about Bellevue Hospital being the first hospital in the U.S., fighting epidemics throughout history all the way back from the 1700’s, Bellevue is Ground Zero, accepting many of the medical transfers. Paul relates Bellevue treating anyone and everyone, including those indigent individuals with no insurance, similarly to America and the Statue of Liberty accepting a diverse population.
Paul spent time speaking with the residents, of whom approximately 50% of the 70 people have been infected with COVID-19.
Today was a long, hard, tough day on the Airway team, Paul responded to 10 codes, and they were able to keep everyone alive. This disease is much worse than initially thought. They estimate that 70% of people who are intubated will end up dying later in the ICU.
There are lots of people in the hospital, sometimes side by side by side. It was a scary and confusing time, all hands on deck.
Teaching point 1.
State of NY released on their data who is dying and who is surviving, what is clear from the data is that that there is a strong genetic component, based on the almost 9,000 deaths, if you are Hispanic you are 2 and a half times more likely to die than a white American. African Americans are two times more likely to die than white Apericans. Paul think that we are going to be hearing a lot more about this being a genetic disease because it’s an RNA virus that gets into the cell and takes over the cell and interacts with out DNA, so it must have a genetic impact.
Teaching point 2
When Paul started his pain practice 12 or 13 years ago, it was about treating every patient like out own Mom or Dad, and what Paul has noticed, is that he is applying that to his practice here in NY for the first time. When he did his residency, he would get the pertinent patient information, name, etc. and he would get out, protecting himself on some level. He was not emotionally affected by it, maybe he cried twice. Whatever the case may be now, perhaps because he is older or wiser, now he is talking to the patient, learning about them, their life, maybe his job this time is to comfort the dying. He has cried every day this week, he is helping them more than medically, just to hold the hand during a scary time is important.
There is a genetic component to this, but also a human element.
Day 4
On day 4 of Paul’s time volunteering to help at Bellevue hospital he speaks of two impactful points during this Pandemic:
Number one is about his own children. Some people who are watching his videos have asked why he would leave his kids at home and go to the frontline in NYC and risk contracting Covid? His response is both empowering and thoughtful: in leading his kids by example he would like them to grow up knowing the importance of helping in this world!
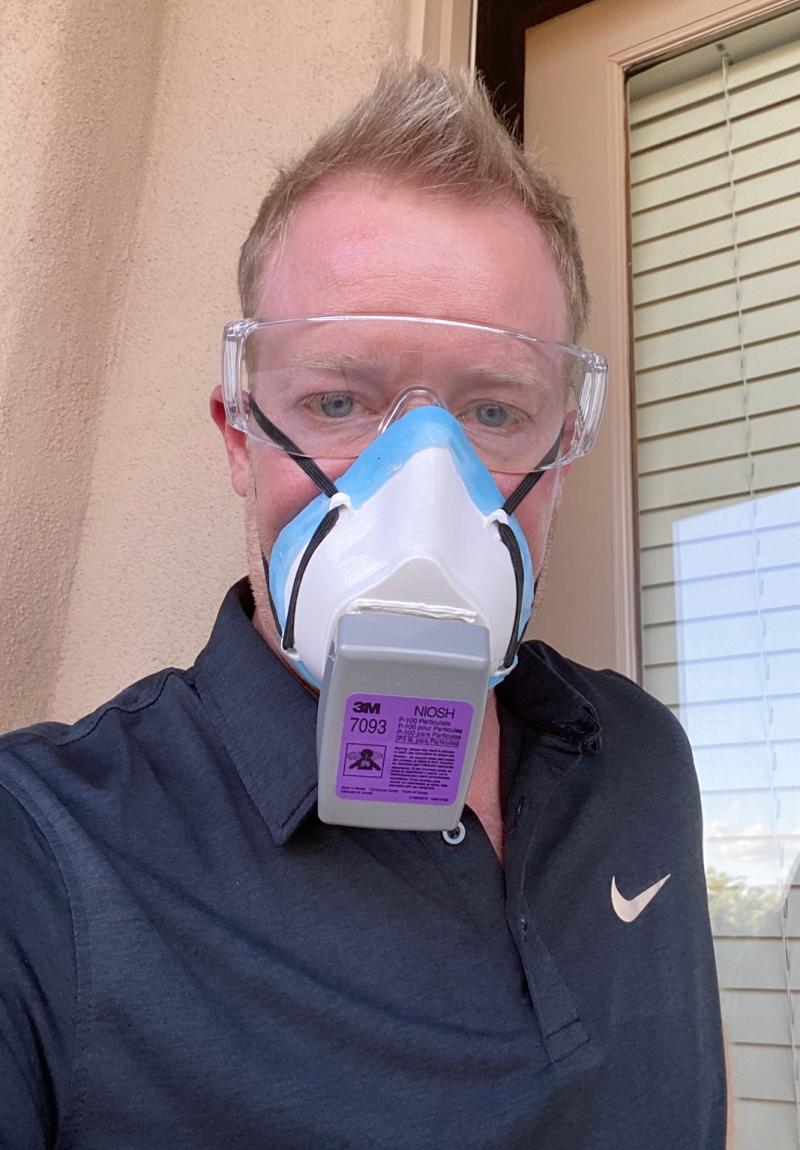
The second impactful message is Paul’s realization and teaching on the importance of logistics and preparedness if this comes to your community. Be prepared logistically with PPE (personal protection equipment) and other equipment.
We are proud to be a helping team helping at this time.
Day 5
Day 6
As much as these videos are difficult to watch, they are also difficult to make.
Today’s video is focusing on positive things: healing and happy moments. Paul is extremely thankful for the military.
Two anesthesiologists from the Navy arrived to help today, they immediately volunteered to help wherever they were needed, and that kind of serving spirit was awesome to see. The Military deployed 200 nurses to help in various positions in NY.
There are many teams at Bellevue: Line team, Airway team, Code team, ICU team (where Paul is managing patients this week) and the Prone team.
On the Prone team, there are 6 people per team and they go around all day and lift patients, flip them upside down and ventilate them on their stomachs, which is very difficult because each patient may have different lines (arterial lines, dialysis, etc.) and it must be carefully done as not to cause the line to slip out or to hurt the patient. The two military men referenced above were going around all day, room to room, because you can’t leave a patient prone all day (it’s 16 hours prone, and 8 hours supine), so these two guys are smiling and sweating because they have to put protective (PPE) equipment, goggles, masks, robes, and gloves and then go and move people around.
Today Paul got to put in the “best epidural of my life” one lady had covid-19 and also horrible trauma, 16 fractures of her ribs on both sides, bilateral pneumothorax (where both lungs collapse), and went through massive surgery, so when she came into the ICU she couldn’t breathe, so they called Paul in as the pain management doctor, to see if he could put in an epidural, a thoracic epidural catheter that he would thread up and infuse medications which would allow her to take a deeper breath. So that is what they did. Paul’s team got suited up and he put in the epidural rather easily, considering he did not have all of the equipment that he usually uses to put them in, This was an epidural that could literally save her life because oxygenation is such a huge issue with these patients who have COVID-19. This was a moment of true happiness for Paul that he has a skill set that can save someone’s life.
Teaching point: The importance of protecting yourself
If you come to work in an environment like this bring your own PPE. Sometimes the hospitals do not have everything you will need when you need it.
Constantly wash your hands, wash your phone, if you touch it, wash it, but try not to touch your phone a lot when you’re in an environment like Covid-19. Create healthy habits when you go home. A study was done in China and revealed that 50% of health care workers who went home had COVID-19 on the soles of their shoes. Paul changes into clean clothes at the hospital, he walks to the apartment complex and takes his shoes off right away, leaving them by the door, he takes off what he is wearing and puts it in a bag to be washed, he washes his phone, he washes his badge, and immediately takes a shower. Do everything you can to protect yourself!
Please send up your prayers for Paul’s 6 patients today. They are all critically ill, close to death, but they have been able to keep them alive. The one from Paul’s previous video who send 50% of his pay to his family in Mexico every week, they depend on him, please pray that he will make it through it. All prayers are appreciated!
Day 7
Today was Paul’s first day off from the ICU in New York, he rested well and did some work on his AZ business.
Paul had some unique experiences near Time Square this morning. His hotel is the Millennium Hotel (provided by Bellevue Hospital and the Millennium Hotel’s combined efforts to support the unpaid volunteers of the Covid-19 pandemic). He decided to get a cup of coffee and take his laundry to be cleaned, however, after walking around for 30 minutes, he found no place open to get coffee or do his laundry. There was no place open to do anything, everything was shut down and the streets were empty. Paul took some picture of the empty street view to illustrate the experience that is unlike anything he has ever had in Time Square before.
Paul was eventually able to find a place that would come and pick up his laundry and he did find some coffee, so it was a pretty relaxing day.
He was able to do a webinar for his patients, an overview of the entire week, a link will be posted soon.
There have been sad stories, thoughtful stories, and hopeful stories from Paul, but today he shares a funny story.
Paul had an intern earlier in the week, and when he went up to do an airway during that week, Paul noticed that this intern was displaying signs of high anxiety, standing next the doors, taking copious notes, pacing back and forth, and Paul was a psychology major in college and enjoys watching people, so he went up to the intern and said that he noticed that he was displaying high anxiety, maybe even uptight. The intern began to protest, but Paul explained that “in the ICU that is not a criticism but actually the highest compliment because your level of anxiety is what is going to help save some of these people’s lives because you are going to double check every number and I’m really proud to have you on my team.”
Teaching point is about life today
Paul has been holed up in a hotel for 7 days, he does not touch people or get close at work. It made him think about being thankful. Be thankful for what you have, family, loved ones, parents. Paul mentioned that he advised his own mother not to leave the house, she has been quarantined for over a month now because of the risk factors. Be thankful for the air you breathe, for relationships, all the things that we take for granted. Now, during these times, we realize how much we have, all our blessings, so be thankful.
Paul is excited to go back to work.
Please continue to pray for Paul’s 6 patients.
Day 8
Paul was glad to be back in the ICU and see that all 6 of his patients, and 2 new ones were still alive, still critical, but still alive. He appreciates your continued prayers.
Paul explains the set up
There are multiple ICUs set up because multiple people are intubated in the hospital. There are COVID positive ICUs where people have the virus and are in intensive care, and then other patients are in ICU’s being treated for typical reasons. Paul is in a level one trauma center in Manhattan, with 20 million people that live in the metroplex.
Paul is working in an ICU where every single patient is positive for the coronavirus, and because of limited space, there are two patients in every room. This is an incredibly different management style than Paul or anyone else has ever done.
To provide an idea of what this looks like, Paul shares this description:
Picture two people in every room with 12 rooms down a hallway, so as many as 24 patients, all with Covid-19. We try to manage the patients from the hall, just to protect everyone, so they set up these intricate systems of drips, and machines, every patient is on anywhere from 2-8 infusions including muscle paralytics, sedations medicines, IV antibiotics, and blood pressure medicines (to keep their pressure up). The tubing is run into the hall, and the doors to the rooms are closed, during rounds it is an incredible sight to see. Walking down the hall you see all of these pumps with all of the nurses managing their patients from outside the rooms, there are really interesting interactions.
Today Paul watched a surgery patient in the Covid-19 unit, and the surgeons were in the room, the scrub nurse was outside of the room, it was just “a sight to behold.”
One of the more difficult things for Paul to watch were the funerals that occur over FaceTime because the family members are not allowed to go into the rooms or even onto the unit. It’s just so high risk for anyone to be there, so when a loved one is near death, social work gets involved and hold the phone as the family members say goodbye. Nobody ever wants to have to say goodbye over the phone, but it is just a blessing for these family members to be able to see their loved one, one last time.
Paul noted good and bad things today. His unit started with about 21 patients, they discharged two, one of whom was Paul’s patient, but two people also died. That is an example of what they are dealing with right now. This is a struggle of life and death every day, winning some and losing some.
Paul explains that when someone is about to be discharged, the hospital always plays the song by Journey “Don’t Stop Believing.” Paul was waiting and excited to hear that song play for one of his own patients when another resident came out and announced that one of his patients had died, it was a somber moment. Within about four seconds, the song started to play, and the joy was sucked out of the moment, overshadowed by another death.
Paul called the mother of one of his patients, he needed verbal consent for treatment from her mother over the phone, she was crying and heartbroken for her daughter, she asked to see her. Paul used an epidural to help the daughter breathe. Paul was unfamiliar with the rules and mentioned that he could have a social worker make the connection between them, but the mother said no, she wanted to see her baby. Paul share that he has five children of his own, he went to ask if he could just do the call with her himself and was given the ok. Paul downloaded an app called Doxicity and sent her a text to connect to the video feed, he worried that this elderly lady may difficulty connecting, but she entered the video meeting right away, so he went over and let her see her baby and she cried and asked lots of questions. Paul did the best he could to explain what was going on. She noticed everything, bandages, vents, monitors, etc. They were on the phone for 20 or 30 minutes.
Teaching point
In this COVID-19 environment there is a way to be able to interact with patients. If you go into your app store and download the app called Doximity, you will have access to two important features. When Paul was calling the patient, or the patient’s family, he would block his phone number, but nobody would answer. When he called displaying his AZ phone number, people still would not answer, but Doximity has a feature where you can label the call, so Paul labelled his calls as Bellevue Hospital and everyone answered. The second feature is a video meeting. It may take 24-48 hours to get set up, but you can send your patients a link via text and they can join you in a video meeting.
Please keep praying for Paul’s 5 patients.
Day 9
Today Paul got to Bellevue hospital a little earlier than usual. Sometimes in the morning there is as much as a 20-minute wait just to get on the elevator. Bellevue is 26 floors high. All of Paul’s patient are still alive, but he asks that we expand our prayers to include two more people that he has been working to save.
Today, Paul wanted to highlight some individuals helping during this pandemic.
He showed a picture of his mentor Ken Sutton, an anesthesiologist who Paul highly regards, teaching and talking to residents. The picture displays notes on a white board for some of the many patients being treated at Bellevue. Paul feels blessed to have known him.
The second picture was of a respiratory therapist who has worked at Bellevue Hospital for 20 years, her name is Lana. She would go and suction out each of the patients, every time she does that, secretions go into the air and she is putting herself at risk, Paul asked her about it and she told him that she loves her job and the chance to help save people.
The third picture is of Chris from Oklahoma. He is a nurse who flew out to help, Paul admired his gear, his mask, and his desire to help save lives.
The fourth picture is for Dave, another of Paul’s mentors who has taught Paul so much about critical care over the years. He helps manage the patients.
The fifth picture is for Nicholas Brimmer, another pain management doctor who was with the Navy.
Anna, chief of ophthalmology at NYU, during COVID-19 she is not doing much surgery, so she has put herself to use helping people become volunteers, helping them get set up with places to stay, and also doing gestures of kindness to help motivate the staff, her little children created some magical PPE necklaces, and Anna has distributed them and shared the tender gesture of her children with many of her coworkers.
Paul’s unit did not lose anyone today, he talked to lots of family members, prayed, and tried to encourage.
Today was the first day that Paul felt scared. One of his older mentors contracted the COVID-19 virus, so Paul and a colleague went downstairs to check on him and the look of fear in the gentleman’s eyes made Paul feel fear too. The mentor remembered Paul from 15 years ago and talked with him, all the while Paul’s heart was pounding. 1/3 of their department has contracted COVID, and 50% of the residents. He started questioning himself after running into a coworker who said that they all were going to get it too.
At the perfect moment, Paul heard an alert on his phone, a friend on Facebook reposted something that Paul put up two years ago about faith, and it was exactly what Paul needed to calm his spirit. Paul showed the picture of the little girl and the lion, explaining that everyone there had been afraid as the lion roared behind a glass wall, except one little girl who went up to the glass, stared the lion in the eyes and said “Calm down.”
Paul shared a biblical scripture from Hebrews 11:1
Faith is the confidence in what we hope for and an assurance about what we do not see.
The girl trusted the glass, just as Paul trusts God. Paul’s fear went away after seeing that post, he believes that God placed him here for a reason. He feels peace that he is exactly where he is supposed to be and doing exactly what he is supposed to do. He has confidence and strength that he is doing the right thing.
Teaching point: Develop great check lists and processes
One of Paul’s mentors said that to be a good intensivist, to keep these patients alive there are 500 separate things that we check every day, sometimes 3 or 4 times a day, he made the point, with 20 patients on the unit and a 500 point check list that’s up to 20,000 things that we have to check today in order to do a good job, and that made Paul think about a couple of concepts, one is Six Sigma for health care (which is a management tool used to improve care for patients by reducing the chance of making errors) and one is checklists and processes.
Paul’s advice for doctors out there, if you get a moment, he would recommend that you read a book called The Checklist Manifesto by Atul Gawande, who is a wonderful physician and writer, his book talks about the importance of checklists, and processes, double checking things and how that leads to better outcomes.
Paul provides his example
When we do a time out in the OR, if we just went in and did cases without organization, we’d probably have an error every 30 or 40 cases, but by doing our time outs and going through specific processes, we can eliminate that down to 1 in 10,000 errors and that is basically what we have to do in the unit, to keep people alive, we have to have a check list, a process, and stick to it.
Please keep Paul and his patients in your prayers.
Day 10
Paul got to work again this morning and was so encouraged to see that his patients are all still alive and being taken care of in the unit. Several of them are near the end of their life, so Paul asks that you continue to remember them and their loved ones in your prayers.
Paul is tired. He has been working 12 and 13-hour days, including working on his day off. His unit got 5 new admissions of various backgrounds: all COVID-19 positive. Paul took on three of these extra patients. He spent a lot of the day running around between them all. One patient really moved Paul emotionally. This man is successful and high ranking in his field. He has been sick for several weeks, and Paul knew that he would need to be intubated with the possibility of never waking up and explained that to this gentleman. 70% of patients will end up dying after intubation. Paul was able to make this patient smile with acknowledging his level of achievement and sharing that his son is interested in his field of study.
There are now 11 patients that Paul has had close contact with, and he is requesting continued prayer for them all.
Paul highlights that his reason for being in NY is not for publicity, but to spread hope and encourage people to make an impact.
He continues to share the stories of others who have come from far and wide to join in the battle of COVID-19.
Paul made a slideshow to share some faces of the people described below.
Rachel Zimmerman is a physician’s assistant, from Atlanta, GA who worked with Paul today. She came because she has ICU experience, she felt helpless staying at home and wanted to come and make a difference. She was scared initially but not anymore. She wants people to know that they do have PPE. She wants her Mom to know that she is safe. Most of the time she wears two masks.
Lauren Hill from Oklahoma City, she felt helpless sitting at home and finally got a call asking for her to come. She feels a little overwhelmed with the number of patients and work to be done, but she is learning so much and helping people. Paul asked her what made her feel the best about what she is doing, and she said that she is so happy to be relieving the workload of people who are tired and have been there for weeks. She said that her family cried when they heard that she was coming.
Bauzo Asabo is rad tech (radiologist technologist) from Harlem who originally lived in Ghana, he goes around their floors all day and takes x-rays to make sure that the lungs aren’t getting worse and making sure that their lines are in the right place. He has had a job at Bellevue for 4-5 months and is proud to fight on the front lines.
Jason from LA is a nurse who felt compelled to come, there was a crisis and he responded.
Devereaux Went is a nurse originally from Jamaica who moved to the United Stated, joined the Air Force, moved from New York and said that when she saw the crisis here, she had to come and help her people, her mom, her family lives here.
Cassie Hampton NP from Dallas came to work as an RN. She is a mother of 4, works 12-hour days at Bellevue and then manages her kids at home through Zoom (video calls) making sure that they are doing their homework and spending time with them.
An RN from NC, previously from Brooklyn, had visible damage on his face from the PPE on his nose face and chin, he was proud to come back to help.
Getting to know the various personalities of the people who have come to sacrifice their own health to make a difference here in NY is one of the privileges that Paul loved about this week.
Funny story
Paul called a patient today and spoke to a family member doing his best to explain what was going on and answering as many complicated questions as he was able. He asked if she had any other questions and she said…” When is the doctor going to call me?” He told her that he was the doctor and said in jest that she hurt his confidence.
This comical moment was shared with other physicians later in the War room, Paul has been in pain management for the past 14 years, so intensive care is not what he does day to day.
Teaching point: Stay healthy
Although the country is talking about reopening and there is excitement, stay healthy. From what they are seeing in the units, the most common comorbidities (multiple health concerns) are diabetes, obesity, hypertension, all of which are controllable with the aid of healthy diet and exercise. COVID-19 may come in waves in the Spring, the Fall, and the Spring again, so this is the time to get in the best shape of your life. Paul has personally lost 20 pounds to be in his best shape. Look into the Mediterranean diet, it is evidence based, with lots of supporting data out of Harvard; it can help you live longer. Take vitamins, exercise, and stop smoking. Set up a wellness check. Be your healthiest version of yourself.
Please continue to pray for Paul and his 11 patients.
Day 11
Since Paul has arrived in New York, between 7,000 and 8,000 people have lost their lives.
Paul looked up the actual number of people who have died, 18,298 people, and he wanted to give you the exact number because every one of these lives matter.
This morning, Paul learned that one of his patients was one of those numbers; he was young. The family told Paul how strong their loved one was and how they were certain that he was going to pull through, he was such a good father, and hard working.
Paul had to continue working to save other lives even though he also felt this loss.
Paul shares some positive updates
A patient’s life was saved thanks to the epidural that Paul put in, they took her inner tracheal tube out and she was able to breathe on her own. He got to speak to her for the first time and he called her mother, who cried and literally screamed into the phone, so grateful. This moment held such joy for Paul that it took away some of the sting from the morning’s loss.
Another win for the day
While Paul and his mentor Dave Rocaforte were next door “vent jocking” (trying to get the exact right numbers to help the patients breathe on their own, even when they are on a vent), a new patient started coding. Paul was so impressed with Dave as he ran into the room where the patient had almost no pulse and his oxygen saturations were in the 30s (and should be 100). Dave rapidly intubated him, gave him an epinephrine and stabilized him.
Dave Rocaforte has been a mentor to Paul for18 years. Paul urges everyone to choose your mentors wisely. Paul likens Dave with the character “House” who knows everything about everything.
Paul played a segment of Dave teaching- a small illustration of his brilliance and the reasons why he is trusted with these patients.
Dave discussed ions and PH levels, stating that the body “endeavors to maintain electrochemical neutrality, so all the positives and negatives (ions) have to counteract and balance”. Dave continues, “When relative proportions change, hydrogen ions come into play” making up the difference which changes the PH level. So the PH is a dependent variable to all the other strong ions, each with it’s own equation, and predictions can be made of what the PH will be when you run all of the other electrolytes through those equations and provide the numbers of the patient. It works and is accurate.
Paul urges people to “pick mentors who are going to push you to be the greatest version of yourself that there is, not necessarily people who will be nice to you and tell you how great you are.”
Teaching point for Doctors
To the physicians, it is not just a lung disease, you will need to come up with Lab tests that look at the overall inflammatory effect on the body, which is how they track it at Bellevue.
Be aware of lymphocytopenia (usually when you get an infection, white blood cells and lymphocytes go up, but this disease crashes the lymphocytes, similar to the way HIV would), so track total or absolute lymphocytes as one of the markers of this disease. Start looking at the lymphocytes as a measure of viral load.
The other things to check daily are D-dimers. D-dimer we look at as a sign of thrombosis like some kind of clot in the body, and your body is breaking down that clot, we usually think it’s like a PE, but with COVID-19, D-dimer is an incredibly good predictor of outcome. The D-dimers are tracked every day, and sometimes we see them as high as 40-50,000 as the virus is attacking the blood system.
We track CPK, the virus’ effect on the muscles and sometimes there are numbers in the 10-20,000s. We track other inflammatory markers too: LDH, ferritin, procalcitonin, IL6, etc.
If you are a physician or PA and you are starting to deal with this, contact me via email or Facebook, I can send you a list of all our lab work. It is a different work up than we are used to in the ICU. We are managing lungs every day to keep these patients alive but also looking at global cytokine storm syndrome, the better we can manage that, the better chance our patients have.
Please keep praying for Paul’s patients, for the work they are doing, and for Paul to stay healthy.
Day 12
Today was a tough day for Paul as he was working on a float team, working with his mentor Ken Sutton, they were doing lines and airways, supporting the unit in any way they could.
Paul slept well the previous night but felt exhausted today. At every opportunity, he found himself wanting to sit and rest, feeling fatigued, where he is typically full of energy.
Paul mentioned his fatigue to Dr. Ostrovsky who brought in the physicians, and he was sent down to employee health, tested, worked up, and sent home. Paul notes that his main symptoms have been fatigue, muscle aches, and later at home he had low grade fevers.
Paul shares his disappointment in the uncertain future and the possibility that his time in NY might be over. He is frustrated not to be at the hospital helping. He stated that what he is experiencing feels like Mono, his throat is sore.
Please pray that if he does get sick that it will be minor, 80% of people have mild symptoms.
Teaching point Medications for Coronavirus
The best data once you have been diagnosed is to take Hydroxychloroquine or Plaquenil, plus Azithromycin (also called Z Pack), a few studies have shown a lot of promise, which is not scientifically validated, but there are a lot of current studies and at Bellevue right now, once diagnosed, they start you on Plaquenil and Azithromycin. If your disease progresses becoming more severe, there are different drugs that can be used.
People ask about taking the two drugs named above prophylactically, and there really isn’t enough data to support that, these are not low side effect drugs, both can affect the heart, and both prolong the QT interval, so using them as a blanket fix for everyone does not make the most sense.
Remdesivir, an antiretroviral which works inside the cell to slow the replication of virus, works really well in petri dishes, but in human studies, there have not been enough to support widespread use. It is being used for compassionate care at Bellevue when people are suffering.
Another drug, Tocilizumab, directly treats the cytokine storm, it has some promise, but there is not enough data for scientific validation currently.
Paul has gotten multiple questions on whether this is like high altitude sickness, and weather Temozolomide or Diamox is useful, and there just are not enough human studies to know, there is some interesting data.
Paul concludes this video with a self-composed song entitled “Coronavirus, You’ll Never Get Me” created while singing with his children.
Please keep Paul in your prayers.
Day 13
Today was Paul’s first day of quarantine, he felt tired, slept a lot, and had more 100-degree fevers. One thing that Paul noted was that his oxygen saturation in his blood was down a little. His test results confirming COVID-19 have not come back yet, but due to the amount of exposure, and having multiple concerning symptoms, he will be treated as though he does have it.
Paul spoke of friendship and relationships and how he was overwhelmed and humbled by the amount of love and support he received. The division chief of ophthalmology stopped by and knocked on the door to deliver about 50 pounds of groceries, fluids, and medications. He received calls from the front desk of his hotel that various people had sent him items and medications. His mentor Ken Sutton sent Paul chicken noodle soup and a pulse oximeter to measure the level of oxygen in the blood (oxygen saturation). Doctors from Oklahoma send Paul medicines, and a local cardio thoracic anesthesiologist sent him medications as well. He cannot thank everyone enough.
Paul shared some pictures of items that he has received, offering assurance to everyone (especially his Mom) that he is not in need of anything and is being well taken care of. He is managing quarantine from his hotel room and appreciates offers that he has received to go to people’s homes if he should get worse, but Paul notes that he felt worse around 10:00am and this afternoon he was feeling better.
Teaching point Check oxygen saturation
Paul does not intend this observation to cause alarm, but he noticed that his oxygen in his blood was much lower than expected, so he wanted to share the video described below.
Paul walked us through what is going on with his pulse oximeter, presuming that he has COVID-19, from 0-100 the pulse oximeter is supposed to be much closer to100. Paul’s reading was close to 90, meaning that he only had about 60% as much oxygen in his blood. Paul finds it interesting that many of the COVID-19 patients are comfortable breathing in the 80 or 90 range. His heart rate shows no distress, sitting and breathing comfortable, he can take deep breaths and the oxygen will go higher.
Paul continues to monitor his own oxygen saturation and notes that he has many friends checking on him, but he wonders if asymptomatic patients who get COVID-19 also have low oxygenation and probably are not using a pulse oximeter at home. Paul is starting to lose his ability to taste, in addition to his other symptoms. He stated that “we need to be checking pulse ox even for minor symptoms.”
Paul wanted to finish this evening highlighting friendship again, for the person who has offered him the most support and encouragement, he played a video that he made for his wife, to show her faith, strength, passion, selflessness, and the incredible contribution to his life and the lives of many others that Janne Lynch has made.
Please continue to keep Paul in your prayers.


Thank you for all that you are doing to care for people with this terrible virus. We are praying for you and for all the patients.
Amanda Noble thank you for your kind words and prayers. We appreciate your support. Ryan, CEO, WorldPix.